Breast Reconstruction Surgery
Overview
Not every woman facing a mastectomy feels the need for breast reconstruction, but for many women it is an important next step in their recovery and overall healing. Breast reconstruction procedures vary depending on the results you desire along with your particular situation and other physical and psychological factors. The best decisions are made when based on medical need and personal desires and expectations.
Mastectomy and Breast Reconstruction
There will be several different physicians who will work hand-in-hand to plan your mastectomy and reconstruction procedure so that you get the best possible result. Your team will include:
1. Breast Surgeon - This general surgeon will perform the biopsy of the breast tumor and the mastectomy.
2. Plastic surgeon - This surgeon specializing in plastic and reconstructive surgery performs your breast reconstruction.
3. Medical oncologist - This physician administers anti-cancer drugs or chemotherapy if required.
4. Radiation oncologist - This physician administers radiation therapy if required
What is a mastectomy?
When cancer is discovered in a woman's breast, a common form of treatment is a mastectomy. A mastectomy is the removal of breast tissue due to the presence of a cancerous or pre-cancerous growth. The decision to proceed with a mastectomy depends on many factors, including the size and stage of your cancer, your particular anatomy and your preferences. You will discuss the mastectomy itself with your breast surgeon.
What is the timing of breast reconstruction?
One of the first decisions you'll need to make if you decide to have breast reconstruction after mastectomy is whether to have immediate reconstruction, which is performed at the time of the mastectomy; or delayed reconstruction, which is performed weeks, months or even years after your mastectomy. You and your surgeon can thoughtfully decide which of these options is best for you.
What are my breast reconstruction options?
There are several ways to approach breast reconstruction:
1. By the use of a prosthesis (a breast implant, either silicone gel or saline-filled).
2. A tissue flap which is a combination of skin, fat, and/or muscle that is moved from your stomach, back, or other area of your body to the chest, where it is shaped into a new breast. A tissue flap also may be used to provide skin or other tissue needed to make up for what was removed at the time of surgery, or changed following radiation treatment.
3. A combination of the two by the use of a tissue expander followed by placement of a permanent implant.
Tissue Expansion Reconstruction
One method of breast reconstruction involves the use of a tissue expander and a breast implant. A tissue expander is a short-term implant with a special valve that is surgically placed under the skin and muscle of the chest, and then gradually inflated with saline over a number of weeks or months to gently stretch the skin. Once the skin is sufficiently stretched, another surgery is performed to remove the expander and replace it with a breast implant.
Tissue Flap Reconstruction
Flap reconstruction is a method of breast reconstruction that uses a woman's own tissue from her back or abdomen to create a breast mound. The tissue flap may be left attached to the blood supply and moved to the breast area through a tunnel under the skin (a pedicled flap)or the vascular supply can be completely detached and the flap moved to the breast area and the vascular supply reattached via microsurgical techniques (a free flap). A pedicled flap is by far the most common flap technique.
Flap surgery creates scars at the site where the flap was taken and on the reconstructed breast. However, flap surgery has the advantage of being able to replace tissue in the chest area. This may be useful when the chest tissues have been damaged and are not suitable for tissue expansion as is sometimes the case following radiation therapy.
Flap reconstruction is most commonly performed using one of two methods: the Latissimus Dorsi Flap, in which skin, tissue, and the latissimus dorsi muscle are taken from the back and tunneled below the skin to the breast area to create a breast mound or the TRAM flap in which skin, tissue, and rectus muscle that are taken from the abdomen and tunneled to the breast area.
It is important for you to be aware that flap surgery, particularly the TRAM flap, is a major operation and requires good general health. If you are overweight, smoke cigarettes, have had previous surgery at the flap site or have any circulatory problems, you may not be a good candidate for a tissue flap procedure. Also, if you are very thin, you may not have enough tissue in your abdomen or back to create a breast mound with this method although an implant can be used to augment either the latissimus dorsi flap or rectus flap reconstruction.
Latissimus Dorsi Flap Reconstruction
During a Latissimus Dorsi flap procedure, the surgeon moves a section of the tissue from your back to your chest to reconstruct the breast. This type of reconstruction also commonly utilizes an implant beneath the pectoralis muscle to augment the newly reconstructed breast.
The Latissimus Dorsi flap procedure typically takes two to four hours of surgery under general anesthesia. Typically, the hospital stay is overnight. You can resume daily activity after two to three weeks. You may have some temporary muscle weakness in your back and shoulder. You will have a scar on your back, which can usually be hidden in the bra line.
TRAM Flap Reconstruction
During a TRAM flap procedure, the surgeon removes a section of tissue from your abdomen and moves it to your chest to reconstruct the breast.
A pedicle TRAM flap procedure typically takes four to six hours of surgery under general anesthesia; a free TRAM flap procedure generally takes longer. Typically the hospital stay is two to five days. You can resume normal daily activity after six to eight weeks. You may have temporary or permanent muscle weakness in the abdominal area.
Use of Implants with Flap Reconstruction
It is important to remember that a breast implant or tissue expander to be replaced with a permanent implant later can be used in conjunction with a tissue flap if the transferred tissue does not provide enough mass or produce the desired results. Depending upon the type of mastectomy performed, sometimes a breast implant can be placed without flap reconstruction or the use of a tissue expander. This is possible only in cases where adequate tissue is left intact and the implant to be placed is relatively small.
In the case where breast cancer only affects a single breast, women with ptosis (sagging breasts) may choose to have a mastopexy, or breast lift, of the opposite breast. This will help to achieve symmetry with the reconstructed breast. Small- or large-breasted women may elect to have the opposite breast enlarged or reduced.
Will breast reconstruction require additional surgeries?
It is likely you will undergo additional surgeries to improve symmetry and appearance - whether or not you have reconstructive surgery with or without breast implants. These additional surgeries may be part of a several-stage reconstruction of the removed breast, or may be to shape the remaining breast to bring it into better balance with the reconstructed one. Most commonly, breast implants are inserted after a space has been created for them using a temporary soft tissue expander that can be placed at the time of mastectomy, or at a later time.
Nipple reconstruction is normally done as a separate outpatient procedure after the initial reconstruction surgery is complete. Because the nipple and areola are usually removed with the breast tissue during a mastectomy, the nipple and areola can be reconstructed as a separate surgical procedure. The nipple is reconstructed with local breast tissues/skin and the areola is usually reconstructed by using a skin graft from another area of the body or from the opposite breast. The area also may be tattooed after sufficient healing to obtain a better color match.
Summary
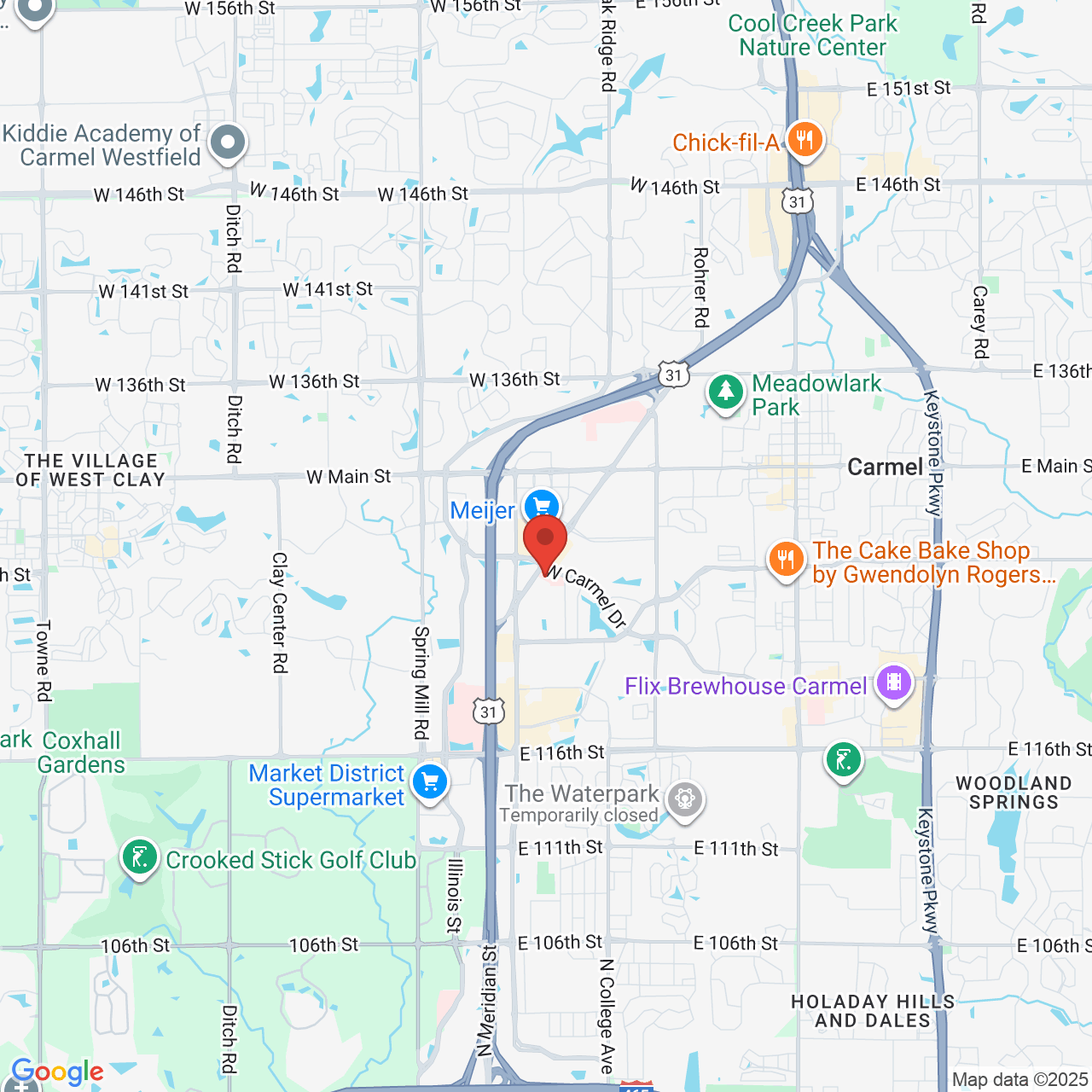
Whether you decide to have breast reconstruction at our Carmel plastic surgery office will depend on your medical condition, general health, lifestyle, emotional state and breast size and shape. You should consult your surgeon to discuss your personal goals for breast reconstruction. For many women, the support and perspective of family, friends, breast implant support groups, and breast cancer support groups can help you make the right decision.
Get Started Today!
Contact us to schedule a consultation. Carmel Cosmetic and Plastic Surgeons provides a supportive environment in which you can feel at ease to discuss your goals. Our physicians, Dr. Elizabeth Grasee and Dr. Debra Bergman, will educate you further on the procedure, evaluate your case, and help you decide the best course of action to achieve your desired outcome. We are committed to guiding you towards a solution that aligns with your personal preferences and maintains your health.